There are several new scientific developments regarding COVID-19 that might be useful to you for navigating the pandemic. All stem from different COVID-19 “story threads” that I’ve written before. So, here is a quick round-up.
Moderna is doing better
What we know: Even though Moderna and Pfizer are both mRNA vaccines, they have distinct micro-differences. The impact of those differences on immune defenses has been up for debate.
New info: Another study confirmed that Moderna induced a better first defense (protection against infection). In addition (and for the first time) we see that it also generated a larger T-cell response (i.e. secondary defense) than Pfizer. This likely impacts downstream outcomes, like duration and strength of protection against severe disease.
Why does this matter? Given this study and previous ones, there should be a preferential recommendation for those over age 50 to get Moderna over Pfizer. This is particularly important for older adults, as they have weaker immune systems.
Reinfections and implications for COVID-19 future
What we know: We have 30+ studies showing that hybrid immunity (vaccination + infection) is strong. However, we don’t know how durable the protection is as Omicron continues to mutate.
New info: A Lancet study assessed the probability of a BA.5 infection (U.S. “summer wave”) after a BA.1 infection (last U.S. “winter” wave). Hybrid immunity was stable up to 35 weeks (8 months). This doesn’t mean reinfections sooner aren’t possible. But, on average, there is a significant pattern.
Why does this matter? The “time” populations are susceptible to COVID-19 will determine the frequency and height of future waves in our “new normal.” This gives hope we’ll eventually see seasonal COVID-19 patterns, like we see with other coronaviruses. This may take a decade, but reprieve is eventually coming.
Vaccines and infections (still) reduce transmission
What we know: Before Omicron we knew that vaccines reduced transmission. Mis/dis-information has sown doubts.
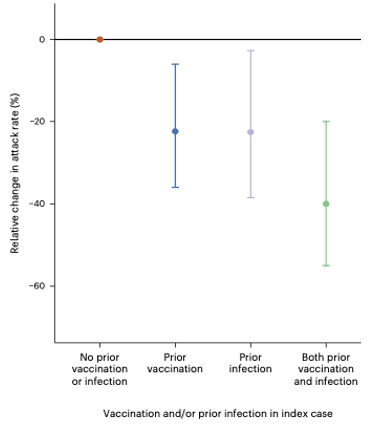
New info: A new study from Nature examined prison systems to assess transmission networks. A COVID-19 vaccine reduced infectiousness by 22% and prior infection reduced infectiousness by 23%. Hybrid immunity reduced infectiousness by 40%. The least infectious cases were those who had been recently vaccinated.
Why does this matter? On an individual level, vaccines still help in ways other than preventing severe disease. On a policy level, timed vaccination campaigns for a variant of concern may make sense until seasonal patterns arise.
There’s a lot of airplanes with COVID-19
What we know: Many studies show the possibility of COVID-19 transmission on planes. However, we don’t know how often COVID-19, on average, is present on planes.
New info: A recent analysis found that among wastewater samples taken from 29 flights from June to Deccember 2022, 28 of the planes had COVID-19 samples. Keep in mind this is not necessarily contagious people, but this is still a lot.
Why does it matter? Keep wearing a mask while traveling if you don’t want to get sick. Especially during surges.
Mask mandates in schools work
What we know: Masks work on an individual level, but the effectiveness of population-level mandates is less understood.
New info: A study from the New England Journal of Medicine compared schools in Massachusetts that kept the mask mandate to schools that removed the mask mandate after the statewide policy was rescinded. Schools that lifted masking had an additional 44.9 COVID-19 cases per 1000 students and staff.
Why does this matter? Mask mandates in large settings, like schools, work. This is important to know now or in future pandemics to keep kids in school.
Novavax
What we know: Novavax looked good in clinical trials, but we haven’t had great evidence on how well it works against Omicron subvariants and in the “real world”.
New info: The first real-world effectiveness data of Novavax’s COVID-19 vaccine was released in a preprint. It doesn’t look great. Those with a Novavax primary series and/or booster were more likely to get an infection than those with an mRNA vaccine.
Why does this matter? As I’ve written before, Novavax is a great option against severe disease if someone doesn’t have the vaccine. But it’s not the silver bullet we are looking for.
Long COVID-19 plateauing after 3 shots?
What we know: Vaccines reduce the odds of long COVID, but we don’t know if the risk continues to decline after each shot.
New info: A JAMA study found that the risk of long COVID decreased with vaccination. But after the third shot, protection against long COVID-19 plateaued. More research is needed, as this is surprising.
Why does this matter? Don’t rely solely on vaccines to reduce your changes of long COVID. It helps, but after a while, not by much.
Bottom line
We are still learning how to live with COVID-19 every day. Yes, science can still help us make better and informed decisions.
You’re now caught up.
Love, YLE
“Your Local Epidemiologist (YLE)” is written by Dr. Katelyn Jetelina, MPH PhD—an epidemiologist, data scientist, wife, and mom of two little girls. During the day she works at a nonpartisan health policy think tank and is a senior scientific consultant to a number of organizations, including the CDC. At night she writes this newsletter. Her main goal is to “translate” the ever-evolving public health science so that people will be well equipped to make evidence-based decisions. This newsletter is free thanks to the generous support of fellow YLE community members. To support this effort, subscribe below:






Thank you. Your posts are always so informative. I especially love your posts on risks of COVID versus risks of other illnesses/accident rates as it helps me make informed decisions for my family.
My 5 year old son was in an accident at school this past week. His finger was shut in one of those heavy, reinforced, quick to close doors that have been installed for safety measures to protect against gun violence in schools. His finger tip was torn halfway off and it broke his finger. The ER Dr said this was happening more often with these doors. He called it before we even told him what happened- he knew it was the heavy, defense doors by how bad the trauma was to his finger. This got me thinking. Our school has spent thousands updating features of the school to make it as safe as it can against gun violence, but has done little this year to stop the spread of viruses in the school. This has even created days when less than half the class was in attendance because of the illness spread (RSV wave). I’d love to have a discussion with the school about a framework of safety inclusive of health safety. Are there any ways to look at risks of say gun violence in schools vs risk of spread that could lead to poor outcomes from COVID and other viruses in school? I’d like to try to make a case for why we should, at the very least, be focused on both areas. Is there a way to compare the risks of both? You were the first person I thought of given your amazing lessons about both COVID and guns- but I also understand if this is too sensitive of a subject.
Excellent article! Thanks so much for all of this data rounded up in one place!